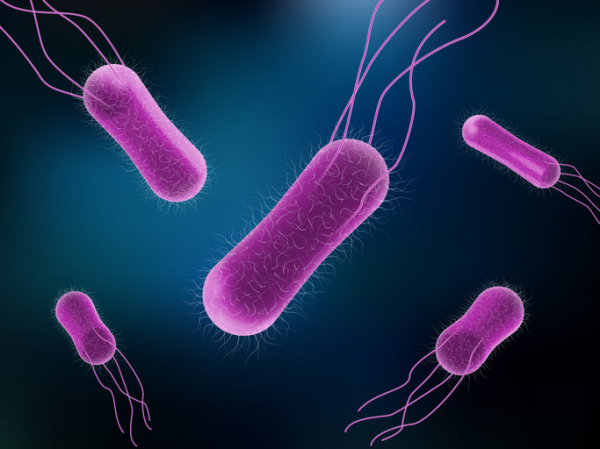
Pop quiz: what is Salmonella? If you’ve ever had a run-in with this bacteria, you know it can cause a food-borne illness called salmonellosis, a form of food poisoning. But you may not know that Salmonella bacteria sicken an estimated 1.35 million people every year in the United States. What’s more, it’s the leading cause of hospitalizations and deaths due to food poisoning.
And Salmonella bacteria can be sneaky — not only by triggering unusual complications, but infecting people in startling ways, says Dr. Elizabeth Hohmann, an infectious disease specialist at Massachusetts General Hospital. One patient she treated showed up with an abdominal aortic aneurysm — a dangerous bulge in the lower section of the body’s largest artery — that looked infected. Testing revealed a culprit some would find surprising: Salmonella.
“It’s just an interesting organism and it can be kind of scary,” she says.
How do people get infected by Salmonella?
Many of the foods Salmonella bacteria lurk in are raw or undercooked. Breaded raw chicken products like nuggets and chicken Kiev are one way it may reach your table. But a variety of foods have been implicated — including organic basil, cantaloupes, ground beef, nut butters, raw cookie dough, eggs, raw or unpasteurized milk, and flour.
Backyard poultry are another source of Salmonella outbreaks. Even small pets such as turtles and frogs, along with dog food, have contributed to multistate outbreaks in recent years.
You can also become infected by handling contaminated food and spreading the bacteria from your hands to your mouth. Additionally, you can spread it to others on your hands or even on your clothes without becoming sick yourself.
“It’s a bug that’s carried in stool and animal feces and is also present in the environment,” Dr. Hohmann says. “So it can set up shop in lots of different inanimate objects, soils, and machinery, especially in moist environments.”
What symptoms can Salmonella cause?
Most of the time Salmonella infection leads to gastroenteritis, usually causing just an upset stomach, abdominal cramps, and diarrhea. These symptoms can start as soon as six hours after ingesting the bacteria. Typically, symptoms resolve on their own within two to three days.
Some people have such mild symptoms they’re barely noticeable. “The classic case might be a college student who eats a burrito from a sketchy place, gets sick for a couple of days, gets better, and doesn’t think anything of it,” says Dr. Hohmann.
Sometimes symptoms are more serious, such as severe abdominal cramping and bloody diarrhea, or unexplained high fever and marked fatigue. These symptoms require a call to your doctor.
How is salmonellosis treated?
Most people will get better on their own without any medicines. Replacing lost fluids by sipping water or electrolyte drinks to avoid dehydration will help.
Call a doctor if you have
- diarrhea and a fever higher than 102° F
- diarrhea that doesn’t improve after three days
- bloody stools
- vomiting so severe it prevents you from keeping liquids down.
Treating the infection with medicine comes with an annoying paradox, Dr. Hohmann says. If doctors decide to prescribe antibiotics, the person taking the medicine may shed the organism for longer than if they were never treated. “Then that person may have the opportunity — either through poor personal hygiene, sex, or working as a food worker — to spread it to others,” she explains. “It’s challenging.”
What complications can Salmonella lead to?
Some people get sicker with salmonellosis than others, with seemingly no rhyme or reason. But certain folks are especially vulnerable to serious infection, including:
- adults 65 and older
- pregnant women
- children under 5
- people whose immune systems are weakened by diseases (such as cancer) or treatments (such as immunosuppressing drugs).
A small percentage of those infected can have Salmonella in their blood, which can spread the infection to other parts of the body such as the urinary tract, bones, joints, or central nervous system (brain and spinal fluid).
And, like Dr. Hohmann’s patient with the abdominal aortic aneurysm, on rare occasions Salmonella can lead to unusual blood vessel complications in people who already have atherosclerosis, blockage of the arteries caused by plaque buildup.
What steps can you take to avoid Salmonella?
We all can take steps to avoid the food poisoning, illness, and hospitalizations that Salmonella exposure can cause.
Dr. Hohmann and the CDC suggest these strategies:
- Using hot water and soap, wash cutting boards or plates on which you cut into raw foods — including vegetables and fruit — before using those surfaces for other purposes. If possible, use separate cutting boards for produce, meat, and fish.
- Refrigerate or freeze foods that are perishable, prepared, or left over within two hours to thwart salmonella growth.
- Always wash hands well with soap and water before preparing food and after contact with animals, using the toilet, or changing diapers.
- If you have a sick pet, take extra care handling its feces and wash your hands thoroughly afterward.
Take additional steps to help more vulnerable people stay healthy:
- Don’t let young children touch high-risk animals, such as turtles, frogs, chickens, or ducks. “And if you’re taking young children to a petting zoo, they should not be petting animals unless you can disinfect their hands immediately afterward,” she says.
- Older adults and those with compromised immune systems should take extra care to wash and cook foods thoroughly.
- People who have had a transplant (such as a kidney transplant) should not keep reptiles or amphibians as pets.
“You hate to make people paranoid, so that we’re washing our lettuce leaves with soap, but it’s worth thinking about these things, particularly if you have people in your household who are susceptible — which is an increasing number of people,” Dr. Hohmann says.
About the Author

Maureen Salamon, Executive Editor, Harvard Women's Health Watch
Maureen Salamon is executive editor of Harvard Women’s Health Watch. She began her career as a newspaper reporter and later covered health and medicine for a wide variety of websites, magazines, and hospitals. Her work has … See Full Bio View all posts by Maureen Salamon
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD Share